What is a Wheeze?
High pitched, musical, whistling sound, monophonic, or polyphonic, that occurs when intrathoracic medium and small airways are narrowed and vibrate due to increased resistance to the movement of air.
Wheezing occurs in large proportion of children under 5 years of age. It is commonly
associated with viral respiratory tract infections.
First Time Wheezing
When wheezing occurs for the first time in an infant it is usually due to acute viral bronchiolitis.
The diagnosis is mainly clinical. X-ray chest may show hyperinflation with air trapping or sometimes it may be normal.
Management of first time wheezer (usually acute bronchiolitis):
· To maintain oxygen saturation and adequate hydration. Oxygen by nasal cannula or hood is given whenever saturation falls below 92%.
· Bronchodilators like salbutamol may be given through nebulizer as a trial initially to assess response in infants who wheeze for the first time, triggered by viral respiratory tract infections. However, in acute bronchiolitis per se it is not effective and not indicated.
Recurrent Wheezing Details of the Symptoms
In a child with recurrent wheezing, detailed history and examination is of paramount
importance. The following questions need to be asked to ascertain a diagnosis of asthma.
· Onset of cough/wheezing—insidious/sudden
· Duration of cough—how many days
· Timing of cough/wheezing—daytime/nocturnal
· Type of cough—dry/wet
· Frequency of cough/wheezing—number of days per month
· Perennial or seasonal
· Symptoms—variable or persistent, whether associated with fever?
· Interval symptoms—symptoms in between the episodes
· Activity limitation—school absenteeism and restricted play
· Triggers—viral infections, smoke, exposure to dust, mold, cat, grass/tree pollen, food, in response to activity/exercise, laughing, crying, etc.
· History of allergy (atopic dermatitis and allergic rhinitis)—in the child/asthma in parents
Documenting airflow limitation: The presence of wheeze one or more times in the past, documented by a physician
Documenting reversibility: Response to beta2-agonist inhalation or documented response to a trial of inhaled corticosteroid (ICS)
The Global Initiative for Asthma (GINA) guideline proposes grouping of recurrently
wheezing patients based on probability of asthma.
Modified Asthma Predictive Index
Modified Asthma Predictive Index is an objective tool used to predict the occurrence of asthma in preschool children.
It is used in children who have 4 or more wheezing episodes in a year. It is said to be positive when at least one major or two minor criteria are present (Flowchart 1.)
Flowchart 1
The mAPI has moderate positive predictive value but good negative predictive value (95%) owever, before confirming asthma diagnosis in any child, particularly in this age group it is important to exclude alternative causes of cough and wheezing.
Clinical features where alternative conditions or asthma mimics are more likely are as following:
· Onset of wheezing in the neonatal period
· Wheezing in infants below 6 months of age
· Nonvariable fixed or persistent signs or symptoms
· Unilateral signs and localized signs
· Wet productive cough, presence of high fever
· Failure to thrive, steatorrhea, and clubbing
· Multiple system involvement and persistent hypoxia
· Poor response to bronchodilators
· Wheezing with dependent edema and/or cardiac murmurs
· Wheezing accompanied by stridor
Differential Diagnosis in Wheezers below 5 Years of Age—Asthma Mimics
All the conditions mentioned in the figure should be excluded by history, examination, and, if necessary, by appropriate investigations.
Investigations in Recurrent Wheezers
If the history is suggestive of typical viral-induced wheezing or that of asthma no investigations are necessary. However, in ambiguous cases with suspicion of some alternative condition certain investigations may be required.
· Complete Hemogram
Eosinophilia may be detected. However, its absence does not rule out possibility of asthma.
· X-ray Chest
To rule out alternative conditions in differential diagnosis.
· Allergy Tests
These may be useful to document allergen sensitization in those who report allergic symptoms on exposure to a particular allergen.
Investigations in Recurrent Wheezers
· Fraction of Nitric Oxide
Fraction of nitric oxide (FeNO) in exhaled air may be used to identify those with eosinophilic inflammation to predict response to corticosteroids.
· Spirometry
Spirometry usually cannot be performed reliably by children under the age of 5 years; other techniques such as forced oscillation technique (FOT) and impulse oscillometry (IOS) are now available at a few centers which can be used in doubtful cases.
Treatment of Recurrent Wheezers
Inhalation treatment is the mainstay in the treatment of wheezing. Inhaled short- acting betaagonist (SABA), usually salbutamol, is used as initial reliever treatment until symptoms subside.
Choice of Inhaler Device
· Till 4 years: Metered-dose inhaler (MDI) + spacer + mask or nebulizer in hospital setting
· Above 4 years: MDI + spacer with mouth piece. Mask should be removed as soon as child can breathe through mouthpiece.
Treatment Plan
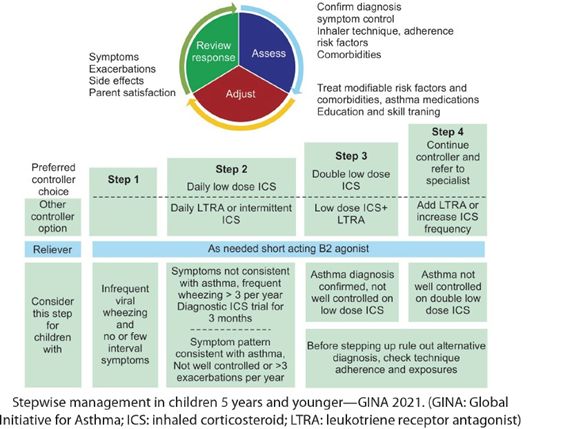
In children under 5 years of age with recurrent wheezing, the following treatment plan is recommended (Flowchart 2).
Flowchart 2: Treatment plan for children under 5 years of age with recurrent wheezing.
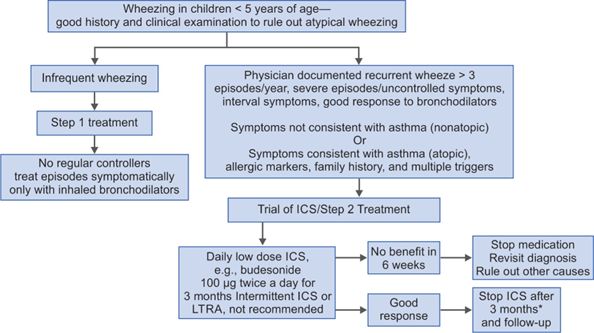
*In children with severe episode/life-threatening exacerbation in the past, it is important to continue inhaled corticosteroid (ICS) for a longer period at a minimum dose that can prevent further exacerbation with periodic monitoring until the child outgrows the symptoms. If no risk factors for exacerbation are present, ICS should be stopped and child followed up for symptom recurrence. ICS can be restarted if symptoms recur.
Step 3 and Step 4 Treatment
In some children, if symptoms are not well controlled after 3 months of low dose budesonide and if diagnosis of asthma is certain then higher step of treatment may be necessary. But before proceeding to higher dose of ICS, the following should be checked:
· Adherence with inhaled medications
· Technique of device use
· Comorbidity
· Ongoing exposure to allergen
If even after correcting all of the above, symptoms persist, then treatment is stepped up to step 3. ICS dose is doubled, e.g., 200 μg of budesonide twice a day for next 3 months.
If child is not well-controlled on this double low dose regime after removing all modifiable risk factors, treatment can be stepped up to step 4. However, such a child should be referred to asthma specialist for further management.
Treatment of Acute Exacerbation (Flare up or Asthma attack)
Exacerbations (flare-ups) of asthma are episodes characterized by progressive increase in symptoms of shortness of breath, cough, wheezing or chest tightness, and progressive decrease in lung function. They are classified as mild, moderate, or severe attack. A scoring system is used to classify and monitor severity of attack.
Doses
· For nebulization—salbutamol 0.15 mg/kg/dose, ipratropium-250-500 µg/dose
· Prednisolone-1 mg/kg/day for 3-5 days
· Injection hydrocortisone 2-5 mg/kg intravenous (IV) 6 hourly or injection methyl-prednisolone 1-2 mg/kg/6 hourly
· IV magnesium sulfate 25-50 mg/kg/dose as slow infusion over 30 minutes
Management of Acute exacerbations
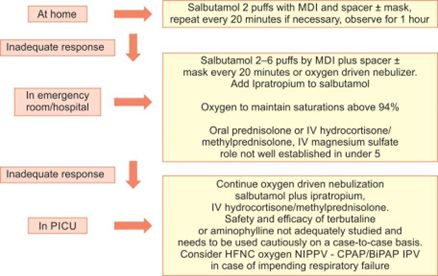
Summary of management of flare-up. (BiPAP: bilevel positive airway pressure; CPAP: continuous positive airway pressure; HFNC: high-flow nasal cannula; IV: intravenous; MDI: metered-dose inhaler; NIPPV: noninvasive positive-pressure ventilation; PICU: pediatric intensive care unit)
Further Reading
· Bush A, Grigg J, Saglani S. Managing wheeze in preschool children. BMJ. 2014;348:1-7.
· Castro-Rodriguez JA. The Asthma Predictive Index: a very useful tool for predicting asthma in young children. J Allergy Clin Immunol. 2010;126:212-6.
· Ducharme FM, Dell SD, Radhakrishnan D, Grad RM, Watson WT, Yang CL, et al. Diagnosis and management of asthma in preschoolers: a Canadian Thoracic Society and Canadian Paediatric Society position paper. Can Respir J. 2015;22:135-43.
· Fakhoury K. (2022). Evaluation of wheezing in infants and children. [online] Available from https://www.uptodate.com/contents/evaluation-of- wheezing-in-infants-and-children. [Last accessed April, 2022].
· GINA. (2021). 2021 GINA Report, Global Strategy for Asthma Management and Prevention. [online] Available from https://ginasthma.org/gina-reports/. [Last accessed April, 2022].
· Moral L, Vizmanos G, Torres-Borrego J, Praena-Crespo M, Tortajada-Girbés M, Pellegrini FJ, et al. Asthma diagnosis in infants and preschool children: a systematic review of clinical guidelines. Allergol Immunopathol. 2019;47(2):107-21.
References
- Bush A, Grigg J, Saglani S. Managing wheeze in preschool children. BMJ. 2014;348:1-7.
- Castro-Rodriguez JA. The Asthma Predictive Index: a very useful tool for predicting asthma in young children. J Allergy Clin Immunol. 2010;126:212-6.
- Ducharme FM, Dell SD, Radhakrishnan D, Grad RM, Watson WT, Yang CL, et al. Diagnosis and management of asthma in preschoolers: a Canadian Thoracic Society and Canadian Paediatric Society position paper. Can Respir J. 2015;22:135-43.
- Fakhoury K. (2022). Evaluation of wheezing in infants and children. [online] Available from https://www.uptodate.com/contents/evaluation-of- wheezing-in-infants-and-children. [Last accessed April, 2022].
- GINA. (2021). 2021 GINA Report, Global Strategy for Asthma Management and Prevention. [online] Available from https://ginasthma.org/gina-reports/. [Last accessed April, 2022].
- Moral L, Vizmanos G, Torres-Borrego J, Praena-Crespo M, Tortajada-Girbés M, Pellegrini FJ, et al. Asthma diagnosis in infants and preschool children: a systematic review of clinical guidelines. Allergol Immunopathol. 2019;47(2):107-21.