Gastrointestinal Bleeding
Hematemesis – Vomiting of blood.
Colour of vomitus depends on the concentration of HCl.
Hematemesis usually indicates bleeding proximal to the ligament of Treitz, because bleeding from the GI tract beyond that, rarely enters the stomach. While bleeding sufficiently enough to producehaematemesis, it is bound to produce melena; less than half of the patients with melena, have haematemesis.
Melena – Black tarry ‘sticky’ stools.
Usually denotes bleeding from esophagus, stomach and duodenum. However bleeding in the GItract down to the ascending colon can produce melena, provided the transit time has been adequate. Blood loss of upto 60 ml can cause a single episode of black stools. Less than 60 ml ofblood loss cause melena for 7 days.
History & Examination
· Ascesshaemodynamic status
· Aspirin, NSAID use
· Alcohol
· Retching, vomiting
· Other sites of bleed
· Telaglectasia – skin & oral mucosa
Estimating the amount of bleed – history and physical examination:-
<500 ml (10% of blood volume) loss- Usually no signs or symptoms. Exceptions are elderly oranaemic patients.
20% blood loss- Gives rise to orthostatic hypotension of 10mm of Hg. Concomitant symptoms include nausea, syncope, light-headedness, sweating and thirst.
25-40% blood volume loss- Can cause profound shock with thready pulse, tachycardia, hypotension, prominent pallor and cold-clammy peripheries.
Investigating a GI bleed :-
Hematocrit- takes 8h to fall by dilutional process. Therefore may not be a good indicator of the amount of bleed. Leukocytosis and thrombocytosis occur with 6h of bleed. Urea rises disproportionately to the Creatinine (because of GI absorption of products of digested blood)
Blood for grouping and cross-matching two pints of blood. If stigmata of CLD are present, LFT, PT,PTT should also be done.
GUIDELINES TO MANAGEMENT OF ACUTE UPPER-GI BLEED
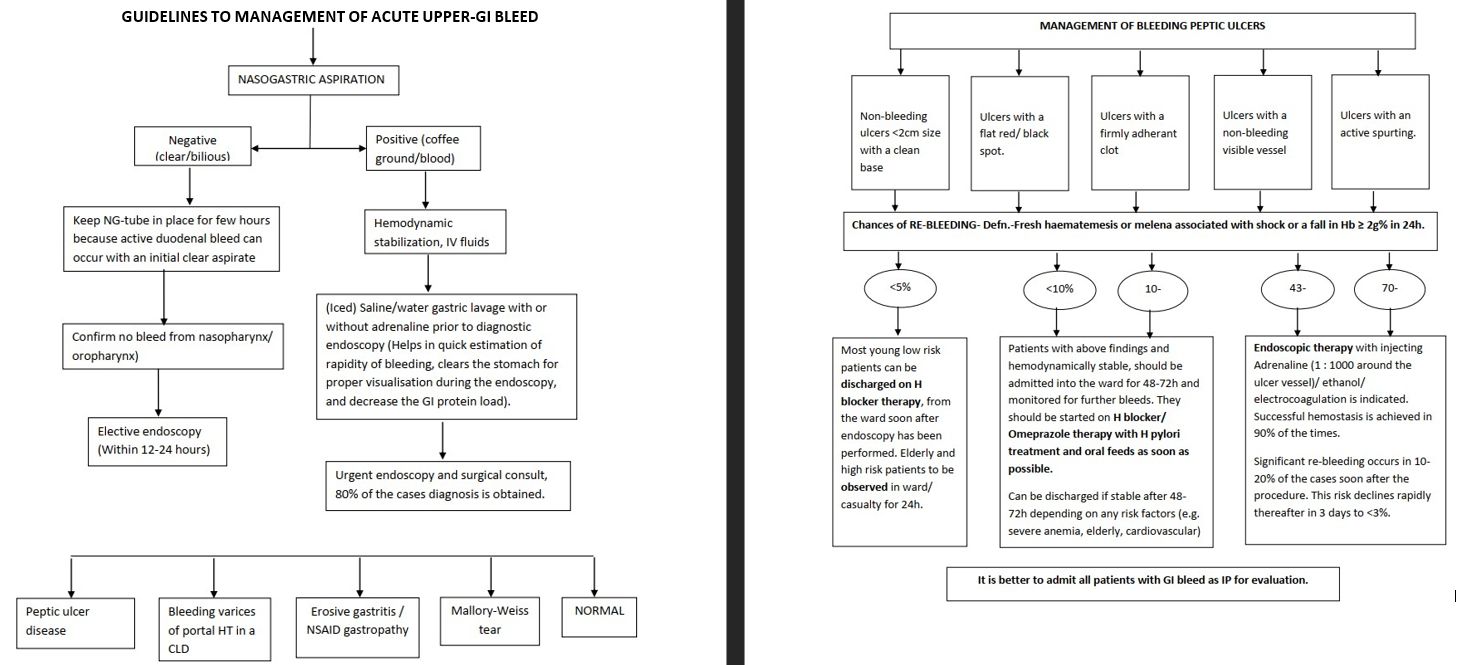
MANAGEMENT OF BLEEDING ESOPHAGEAL/ GASTRIC VARICES
Remember : Patients with varices and portal HT may be in 20-56% of the cases bleed from a non- varicealsource.
Independent Clinical/ Laboratory risk factors associated with non-variceal acute upper GI bleed
· Age more than 60 years
· Severe medical/ surgical co-morbid conditions
· Inpatient hemorrhage (admitted for some other medical/surgical condition)
· Persistanthaematemesis, hematochezia, red NG aspirate
· Persistant hypotension/shock
· Transfusion of >6U of RBCs required during one episode of bleeding
· Re-bleed from the same lesion
· Severe, co-existing coagulation/platelet disorder.
MANAGEEMENT OF BLEEDING ESOPHAGEAL/ GASTRIC VARICES
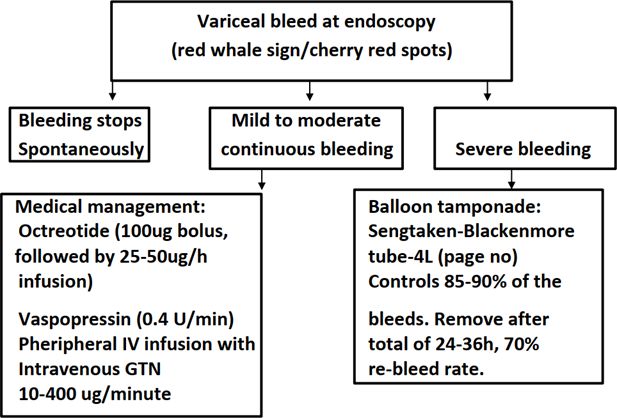
Method of insertion and removal of Sengstaken-Blakemore tube:
1. Empty stomach by suction at endoscopy.
2. Pass down a cooled, 4 lumen SB-tube (Cooling the tube stiffens it and allows easy passage ofthe tube without curling in the nasopharynx.
3. Maintain oral suction. Check position of tube in stomach by air injection and auscultationover the epigastrium.
4. Inject 500-200ml of air/saline into the gastric balloon. Withdraw till resistance felt againstthe gastric fundus. Should be 30-40 cm from the incisors. Tape the tube in place.
5. If bleeding continues, inflate the Esophageal balloon to 30-40 mm of Hg pressure with air.Double clamp the balloon tubes.
6. Maintain a constant low suction of 5-10mm of Hg at the esophageal luminal tube anddependant continuous drainage at the gastric luminal tube.
7. Check position of the tube with Chest X-Ray.
8. If bleeding continuous, question diagnosis, add a traction force of 30gm to the tube and takeX-Ray for confirming position of tube.
9. If at anytime respiratory distress arises, deflate both tubes completely and remove tube assoon as possible.
10. Remove tube after total of 24-36h or 12h after bleeding stops. Deflate the esophageal balloon first, if re-bleeding does not occur, remove tube after 12h, if re-bleed occurs, re-flatethe esophageal balloon. Chances of re-bleed after removal of SB-tube is very high (70%)
EROSIVE- GASTRITIS/ NSAID ABUSE
Most often settles with withdrawal of the offending drug and IV anti-secretory therapy withor without treatment for H.pylori. This is not amenable to endoscopic therapy.
MALLORY-WEISS tear
May or may not require endoscopic injection therapy.
NORMAL AT ENDOSCOPY
Visceral angiogram is indicated if there is active bleeding of >1ml/min in the absence of any structural lesion on endoscopy. For bleeding of lesser extent, colonoscopy is the best option;vascular malformations are the most common. For younger patients consider radio-nucleideTc99-sulphur scan for Meckels’s diverticulum.
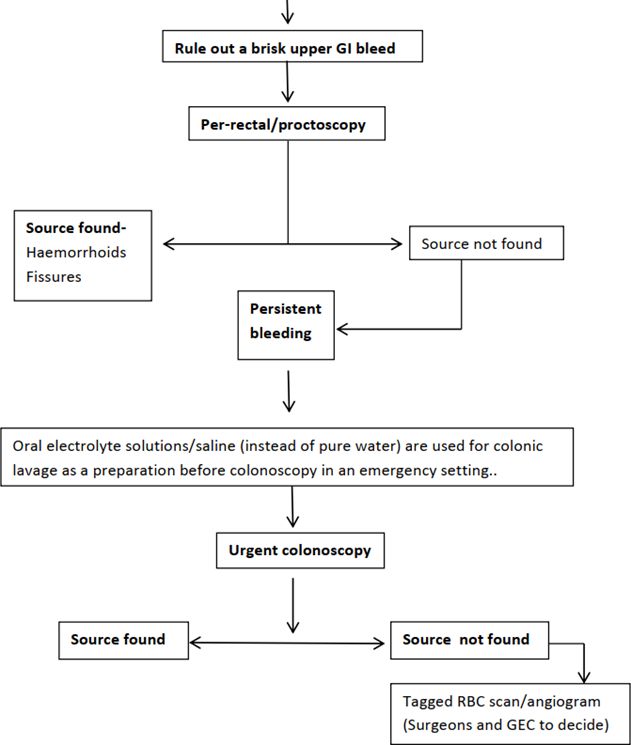
LOWER GI BLEEDING :-
Hematochezia – Fresh bleeding per rectum
Bleeding beyond the ligament of Treitzcan cause this. However brisk bleeding proximal tothis eg. Esophageal varices, can also give rise to hematochezia because of shortened GI transit time.
APPROACH TO BLEEDING FROM THE LOWER GI TRACT
OCCULT GI- BLEED
Occult GI bleeding :-Normal occult bleeding from GI tract is 0.5+/0.4 ml/day (maximum 1.5 ml/day).It does not vary with age or sex. GI bleedingupto 200ml/day can remain as occult.
Detected by ‘hemospot/ ‘GUAIAC’ test in our laboratory which has a sensitivity of 0.5 ml/dayfor colo-rectal bleeding and 10-20ml/day for esphago-gastro-duodenal blood loss. The test detects hemoglobin peroxidase. False-negative test can arise due to ingestion of 500 mg of Vitamin C daily.Aspirin 80-325mg PO/day does not explain occult GI bleeding therefore is not a cause of false- positive result. Should be tested on a high fibre, low-meat die, off all NSAIDS and Vitamin C. Alwayssample 3 stools because of GI malignancies can bleed episodically. More than three sampling reduces the specificity of the test.
Stool for occult blood(SOB), being positive, is a matter of serious concern. It should be followed by an endoscopic evaluation for structural lesion in the GI tract. Patients on NSAIDS and Aspirin therapyare also not excluded from this because there are equal chances of GI malignancy in them and the general population if SOB is positive. (Daily Aspirin therapy is unlikely to cause SOB positive)
Other investigationsto be carried out are, Haemoglobin, MCV, peripheral blood smear (tests foranemia evaluation). Stool for ova, cyst and parasites.
Flow chart for investigating a case of occult GI bleed
(Please order investigations onlyafter discussionwith the consultant) Investigations can be discontinued at any stage when a possible cause for the SOB is detected.
References
No references available