Fluid And Electrolyte Disturbances
1. BODY FLUIDS DISTRIBUTION OF BODY FLUIDS
THEREFORE, IN A 60 Kg MAN TBW=36L (60X0.6)
· DAILY FLUID ORDERS :-
QUANTITY :Normal individual, NPO, maintenance order. 100 ml/kg body weight x first 10 kgs + 50 ml/kg x next 10 kgs + 20 ml/kg thereafter (More useful for children)
For adults, about 3 litres of IV fluids, equally divided between NS and 5% glucose) Daily requirements of
· Potassium= 60 meq (4.5 KCl)
· Magnesium = 8-20 meq (1-3 of MagSO4)
· Na=100 meq,
· Glucose (To reduce catabolism of proteins by half) = 100-150g (2 litres of 5% Glucose).
· Proteins 40g/day
Type of fluid :Usually a balance of NS & 5% Glucose.
For post op 1st day only dextrose…… 2nd day to 3rd day introduce DNS into fluid order. After 3rd day, usual orders.
Supplement potassium if <3days of NPO.
· Volume excess…..Look for increase in weight, pedal edema, ascites, raised JVP, lung basecrepts.
….................. Causes CCF, nephrotic syndrome, cirrhosis, renal failure.
· Volume depletion…..Look for weight loss, excessive thirst, dry mucous membranes,tachycardia, orthostatic hypotension, shock.
……….. Causes vomiting, diarrhea, diuretics, renal (salt losing) disease, DM, DI, excessiveinsensible loss, inadequate oral intake.
· Evaluation…..
Investigations :- Electrolytes, blood urea nitrogen, creatinine, glucose, urine spot sodium,potassium.
INTERPRETATION OF THE FOLLOWING :-
· Serum Osmolality = 2x(Na+ K (meq/L)) + Glucose, 18 + Blood Urea, 6 (MG/DL)
NORMAL = 285-305 mosm/kg
· Urine spot sodium > 20 meq/ l is consistent with renal salt wasting. (Diuretics, ACEI, hypoaldosteronism, salt losing nephropathy.) When less than 10 meq/L it means avidconversation of sodium to comepensate for extra renal losses.
· Correction…..
· Goal is to restore normovolemia
· Fluid should be as close in composition as the fluid lost.
· Monitor weight daily, look at cumulative balance, maintain intake-out put charts.
· In shock/or during large volume replacements, central venous line is mandatory
· Look for signs of overcorrections (JVP, basal crepts, anasarca)
· Mild volume contractions, replace by mouth.
· More severe requires IV therapy. Individualize therapy ; most often it is the ‘blanket protocol therapy’ that harms the patient.
· Amount and type of fluid is determined by serum sodium values.
· With haemorrhage, anemia, might need volume replacement with blood or colloids.
· Quantity of fluid depends on
§ Deficit to start on
§ Maintenance needed
§ Ongoing loss
1. ELECTROLYTES
SODIUM
1. HYPONATREMIA (SERUM SODIUM < 135 meg/L)
CORRECTION:- (17.5meq = 1gm. 1000 ML of NS has 9 gms of sodium 154mmol/lt)
· REPLACEMENT = BODY WT. X 0.6 X (130- SERUM Na) (Sodium is replaced for all the compartments, and therefore in the equation 60% of the body weight is considered thoughthe intravascular volume is only 5% i.e. all the compartments are in equilibrium due to osmotic drive and the major ion involved is sodium).
· The plasma sodium concentration should not rise by more than 10-12 mmol/l/24hr or >25mmol/l/first 48 hours.
· When it is a fall known to have occurred within 12-24 hours, it is safe to correct at a fasterrate than if hypernatremia is more chronic.
In the Depletional form……. Oral/IV Correction
· If mild, asymptomatic ….. Oral Salt
· If symptomatic / severe …… IV
· Fluid replacements to be corrected over 48-72 hrs.
· Fast sodium correction can cause seizures and permanent neurological abnormalities (Central pontine myelinosis- The neuronal response to an extracellular increase in osmolality (and therefore to prevent the outflow of intracellular water) is to break up its
· proteins into ‘IDIOOSMOLES’ (smaller particles over a period of time) which increase sodiumand fluid at this stage can cause cellular swelling due to influx of water into the cell owing toits higher osmolality – therefore causing cell damage. (a.k.a. osmotic demyelination syndrome ODS)
· Total deficit is calculated by using the above formula
· Half of this is given in 1st 8-12 hrs, followed by the rest in over next 12-24 hrs.
In the dilutional form restrict fluids, cautious use of diuretics
· In emergency (like seizures), use 3% saline for correction (same formula as above)
· Correct over a duration of 48-72 hrs.
· Change in serum sodium = (Na I – Na S) (Total Body Water + 1) NaI = Sodium Conc. In Infusate
Na S is Serum Sodium Conc.
Na concentrations in NS = 154 meg/L Na conc. in RL = 130meg/L
Na conc. in 3% saline = 513meg/L
In the SIADH type….
1. Dilutional hyponatremia i.e. plasma hypo-osmolality proportional to the hyponatremia
2. Urine osmolality greater than plasma osmolality (usually)
3. Persistent high urine sodium (>50 mml/l)
4. Absence of hypotension, hypovolemia and edema forming states
5. Normal thyroid, renal and adrenal functions
· In emergency, use hypertonic saline as above
· Restrict fluids to 500-800 ml/day, increased salt intake
· Demeclocycline 600-1200 mg/day
· Lithium
·
Note : Hiccups is a common manifestation of hyponatremia. CF- CNS mainly – alt sensorium
1 level tef = 5 gm Na = 68 M Eg of salt (Na Cl)of hyponatremia.
HYPERNATREMIA
(SERUM SODIUM>145meq/L)
Clinical approach to HYPERNATREMIAS
Investigations:- Ask for Na, K, Ca, Mg and Phosphorus
ALWAYS ASOCIATED WITH HYPEROSMOLALITY
CAUSE-IATROGENIC HYPERTONIC SALINE THERAPY, WATER DEFICITS
TREATMENT:-
· FLUID TO BE REPLACED IS CALCULATED BY-
· WATER DEFICIT=0.6 X WT X (OBSERVED Na- EXPECTED Na)/ EXPECTED Na
· TYPE OF FLUID ½ NS, ¼ NS, 5% DEXTROSE
· RATE OF LOWERING SODIUM SHOULD NOT BE > 2mmol/L/h
DISORDERS OF POTASSIUM BALANCE
· Predominantly intracellular ion (Only 2% is in ECF)
· Normal range 3.5-4.5 meq/L.
· Normal daily requirement = 60meq
· Normal K1/K (potassium concentration intracellular/extracellular) ratio = 35-40
/ 1
· 1g KCl = 13meq of K
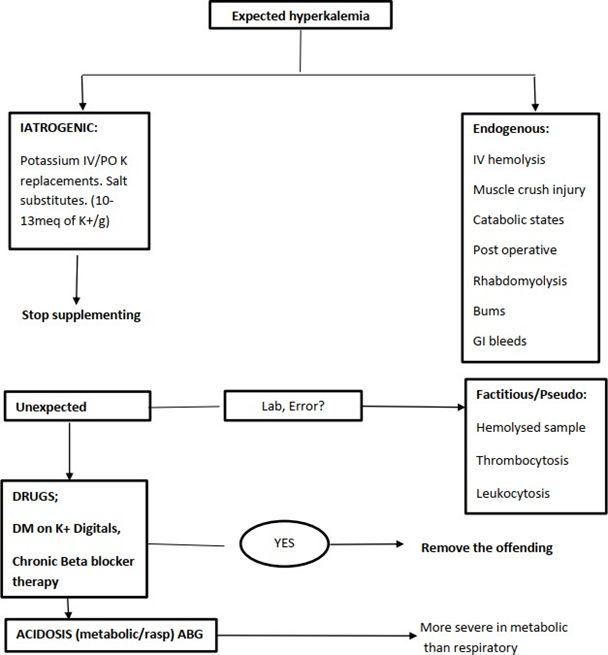
HYPERKALEMIA
Defn: >5.0meq/L
An approach
CLINICAL FEATURES
Paresthesias, ascending muscle weakness, Muscle weakness is due to a rise in the thresholdlevel of stimulus.
ECG :- Changes in hyperkalemia.
In chronic cases, there maybe no ECG changes even at levels of 7.5meq/L.
Cardiac toxicity can therefore occur in them without any premonitory ECG changes, therebygoing into direct VF. Thus treat all hyperkalemias > 6.0meq/L.
ECG changes: Corresponding Se. K+ levels.
Tenting ‘T’ waves, ST depression. 5.5-6.0meq/L
PR and QRS widening 6.0-7.0meq/L
‘P’ wave flattening
Widening of QRS and PR 7.0-7.5meq/L Atria conduction ceases, ‘P’, wave disappears
QRS merges with ‘T’ wave, ‘SINE’ wave pattern. >8.0meq/L (Error of misdiagnosing VT)
Ventricular asystole/fibrillation >10meq/L
TREATMENT FOR ACUTE HYPERKALEMIA
(mostly by inter compartmental shifts)
· Do not use Calcium for Digitals induced cardiotoxicity with hyperkalemia
NON-EMERGENCY THERAPY
(mostly by getting rid of the potassium from the body)
Modality | Mech.Of action | Duration | Prescription |
Loop diuretic | Renal Excretion | 0.5-2h | Furosemide, 40-160mg, IV +/- NaBicarb |
Kayexalate |
Ion exchange |
1-3h |
PO 15-30g in 12.5% Sorbitol (50- 100 |
(Sodium polystyrene sulphonate) |
| ml). Rectal, 50g in 20% Sorbitol |
Hemodialysis | 48h |
|
Peritoneal dialysis | 48h | Fast exchange, 3-4L/h |
TREATMENT OF CHRONIC HYPERKALEMIA
· Low potassium diet (<60meq/d)
· High carbohydrate diet (if not diabetic)
· Avoid drugs causing hyperK+ e.g. ACEI, K+ sparing diuretics, Beta blockers,PG synthetase inhibitors, Heparin.
· Diuretic (Thiazides/ Furosemide in renal failure)
· Sodium bicarbonate orally to increase blood pH
· Exchange resins
HYPOKALEMIA
Defn:<36meq/L An approach…
Hypo kalemic PP (periodic paralysis) :- (Autosomal dominant) Normotensive, Hypokalemia. NO kaliuresis.
RTA I and II :- Normotensive, Acidosis, hypokalemia, kaliuresis, hyperchloremic.
Bartters’s :- Normotensive, Alkalosis, hypochloremic, hypokalemia, kaliuresis, Increased Renin and Aldosterone. Responsive to therapy with all potassium sparing diuretics.
Liddle’s :- Hypertensive, decreased Renin and Aldosterone, Responsive only to Amiloride andTriamterene. Non-responsive to Spironolactone.
Potassium depletion without Hypokalemia :- Digitals therapy
Untreated essential HT Non-oliguric CRF
CLINICAL FEATURES
· No symptoms at >3.0 meq/L
· Muscle weakness :- Explained by the change in the Ke/Ki ratio due to intracellular potassium depietion, thereby making the resting membrane potential more negative.
This is in contrast to the mechanism of muscle weekness in Hyperkalemia. Investigating a hypokalemia
· All other electrolytes as mentioned in the flowchart.
· ECG changes :-
1. Flattening of ‘T’ waves
2. ‘ST’ depression
3. Emergence of ‘U’ waves
4. ‘PR’ prolongation at <2.0.Omeg/L
5. Various arrhythmias :- APCs, VPCs, SVTs, high degree AV blocks,VT,VF.
· Chronic hypokalemia produces metabolic alkalosis.
TREATMENT OF HYPOKALEMIA
There is very poor correlation between total body potassium and the serum potassium. The following graph depicts the derived correlation between the two in a 70kg man.
· Total body potassium (3470)= intracellular potassium (3400 meq)+ extracellular potassium(70 meq).
· ACIDOSIS and ALKALOSIS shifts the curve in the above mentioned directions.
· Between 2.0 meq/L of serum concentrations, the potassium deficits is much more for asmall drop in serum concentrations.
· Above 4.5 an increase in serum potassium of 1 meq/L is associated with an increase of 100meq of total body potassium excess.
· In other words the potassium depletion has to be thrice as large than the potassium excess to give rise to a significant (1meq/L) change in the serum concentration of potassium.
· This difference is due to a large pool of intracellular potassium, which can replenish extraceilular stores when potassium is lost. The Ki/Ke( which is fairly constant between 2.3and 4.5, i.e. 35-40:1) ratio decreases whenever there is an excess of potassium. This ration of distribution also is low when potassium is given as a correction for hypokalemia. A decrease in ki/ke ratio increases the chance of cardiac arrest in asystole.
· Therefore, rates of replacement should never exceed 40 meq/h/l. A rate of replacement of 0.75 meq/kg over 1-2 hours increases the S. potassium by 1.0 to
1.5meq/L slowlydistributing at a ratio of Ki/Ke of 12-15:1.
· In case of REFRACTORY hypokalemia, correct magnesium (Intravenous magnesium SO4), change the infusing fluid to mannitol from dextrose/saline (to reduce the intracellular transport of the ion when given with dextrose and to prevent kaliuresis which proportionallyincreases with the distal tubular sodium load).
· THE BEST GUIDE TO REPLACEMENT THERAPY IS SERIAL MONITORING OF THE SERUMPOTASSIUM.
Preparations :- Oral syrup KCI (5ml=4meq of potassium)
InjectionKCI
For potassium chloride, 13meq=1g
References
No references available